The rapid rise of digitalization in healthcare has made data migration in healthcare a critical priority for hospitals, insurers, and providers worldwide. As electronic health records (EHRs), patient portals, and connected devices generate vast amounts of sensitive data, organizations are under pressure to modernize their IT systems for better efficiency, compliance, and patient outcomes. According to HIMSS, “by 2025, 80% of healthcare providers will have migrated to cloud-based systems,” underscoring the urgency of seamless and secure data migration.
But healthcare data migration is not the same as generic IT migration. It involves moving complex datasets such as patient histories, billing details, imaging records, and regulatory information, all while ensuring compliance with HIPAA, GDPR, and other industry standards. Done right, it ensures continuity of care, prevents data silos, and sets the foundation for interoperability across healthcare ecosystems.
In this blog, we’ll explore what healthcare data migration entails, why it matters, best practices for success, real-world case studies, and the future trends shaping the industry.
Key Takeaways
- Healthcare data migration has become essential as digital health systems grow and legacy infrastructure can no longer support scale, compliance, or advanced care delivery.
- Healthcare migrations are complex because they involve sensitive clinical data, mixed formats, and strict regulations that directly impact patient safety.
- Most migration failures stem from poor data quality, interoperability issues, compliance risks, system downtime, and low user adoption.
- Successful migrations follow a structured approach with data assessment, cleansing, phased execution, strong security, and clinical involvement.
- Cloud platforms, AI-assisted mapping, and targeted RPA use improve migration accuracy, speed, and long-term system reliability.
- Kanerika helps healthcare organizations modernize securely by delivering compliant, low-disruption migrations that enable analytics, interoperability, and AI-driven care.
What Is Healthcare Data Migration and Why Is It Important?
Healthcare data migration involves the process of transferring patient data, electronic medical records, electronic health records, billing data, and clinical data from one system to another. It occurs when hospitals, clinics, and insurers upgrade from outdated systems to modern-day digital platforms. This process is important since patient data must remain accurate and accessible throughout the change.
There are three major types of healthcare data migration:
- Storage migration involves moving data from old storage systems into new hardware or cloud storage for improved scalability and resilience
- Application migration moves data from one application to another, such as moving from an older EMR to a new EHR system, such as Epic or Cerner
- Cloud migration involves moving healthcare data and applications from on-premises to cloud-based environments such as AWS HealthLake, Microsoft Azure for Healthcare, or Google Cloud Healthcare API
Healthcare data migration is not a simple task like a generic IT migration. The data is highly sensitive, diverse, and mission-critical. Healthcare systems handle both structured data, such as lab results, and unstructured data, such as medical images, prescriptions, and doctors’ notes. Accuracy is important, as even small errors can affect patient safety and treatment outcomes.
Compliance with regulations adds another layer of complexity. HIPAA in the United States and GDPR in Europe have strict requirements for privacy, security, and data handling. A breach or poor handling can result in hefty fines, reputational damage, and loss of patient trust.
Healthcare data migration is not simply a process of transferring information. It is about maintaining data accuracy, security, accessibility, and compliance, and supporting continuity of care.
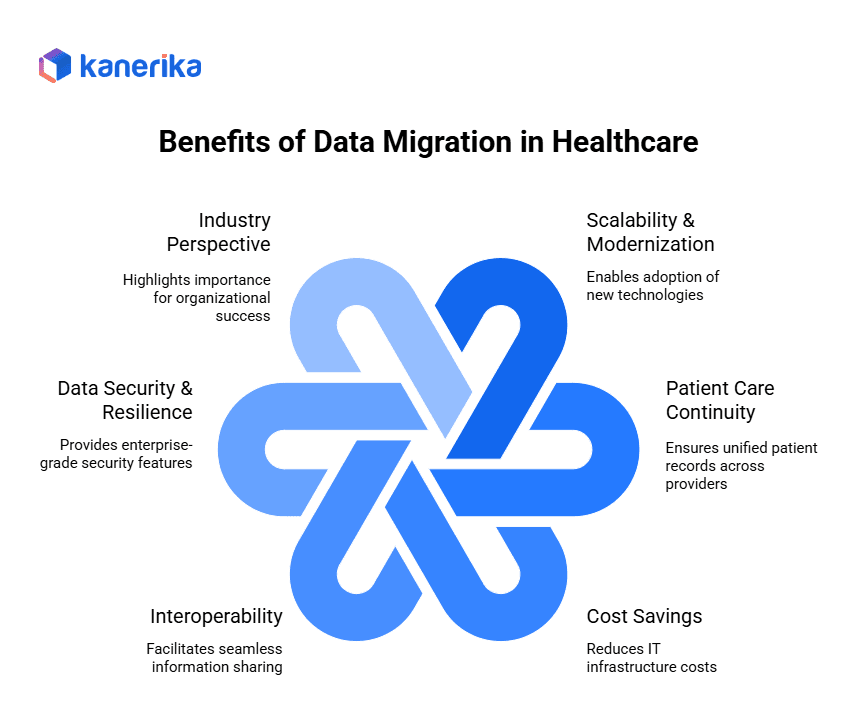
Why Healthcare Data Migration Is Important for Modern Healthcare
Healthcare data migration matters for several important reasons. It affects patient care, operational efficiency, and organizational success.
1. Scalability and Modernization
Healthcare organizations are dealing with massive data growth. Electronic healthcare records, medical imaging, IoT devices, and patient monitoring systems all generate vast amounts of data. Legacy infrastructure handles this volume poorly. It creates bottlenecks that slow clinical workflows and reduce the ability to perform analyses.
Modern cloud-based platforms provide almost unlimited storage space and computing power that scales with demand. This scalability lets healthcare organizations implement new technologies like AI-powered diagnostics, predictive analytics, and telemedicine. They no longer have to worry about infrastructure limitations.
2. Improving Patient Care Continuity
Data migration creates unified patient records. These records track patients across diverse healthcare providers and treatment settings. When emergency departments, specialists, and primary care physicians have immediate access to complete medical histories, they make better treatment decisions. They avoid dangerous medication interactions or duplicate procedures.
Seamless data availability helps reduce treatment delays and achieve better patient outcomes. This matters especially for chronic conditions where coordinated care is required between different providers and specialties.
3. Cost Savings with Cloud-Based Solutions
Healthcare organizations save a lot of money when they migrate from expensive on-premises infrastructure to cloud platforms. They eliminate hardware maintenance costs, reduce the need for IT staffing, and enjoy the economies of scale that cloud providers offer.
According to recent industry analysis, healthcare organizations can save 20-40% on IT infrastructure costs. They improve system reliability and performance through strategic cloud migration initiatives.
4. Enabling Healthcare Provider Interoperability
Data migration to standardized cloud platforms offers hassle-free sharing of information. Hospitals, clinics, laboratories, and specialists can all easily share information. This interoperability removes data silos that previously made it difficult to deliver comprehensive patient care.
Standardized data formats and APIs enable different healthcare systems to communicate with one another. Care networks form that provide improved patient outcomes. Administrative overhead and duplicate testing are reduced.
5. Security and Resilience of Data
Modern cloud platforms offer enterprise-level security features. Encryption, access controls, and threat monitoring go far beyond what most healthcare organizations can implement on their own. Automated backup and disaster recovery capabilities ensure patient data is always available, even in the event of system failures or cyberattacks.
Cloud providers spend billions of dollars on security infrastructure and compliance certifications. This gives healthcare organizations access to security infrastructure that would cost them tremendously to build themselves.
6. Industry Perspective
Healthcare IT leaders know how important data migration is to their organizations’ success. Healthcare CIOs consistently rank data consolidation and cloud migration among their top priorities. These priorities help them better deliver patient care and increase operational efficiency.
The shift from on-premises, fragmented systems to integrated cloud systems is critical. It allows healthcare organizations to focus on healthcare rather than technology management.
Challenges of Healthcare Data Migration
Healthcare data migration comes with several significant challenges. Organizations must navigate these carefully.
1. Data Quality and Inconsistencies
Healthcare data is typically distributed across multiple legacy systems. EHRs, lab systems, imaging platforms, and billing tools all contain patient information. Often, these systems hold information in different formats. This leads to duplicates, missing fields, and inconsistent clinical codes.
Industry reports state that nearly 60% of healthcare organizations cite poor data quality as the main obstacle in the migration process. This also increases the risk of data loss and clinical inaccuracies.
2. Mismatch in Interoperability and Standards
Many older healthcare systems were not designed to meet modern interoperability standards. HL7 FHIR and consistent ICD-10 mappings did not exist when these systems were built. As a result, data transformation becomes complex and time-consuming.
Studies show that over 40% of hospitals still run partially interoperable systems. Validation and data exchange with an accurate system remain major obstacles during migration.
3. Compliance and Data Privacy Threats
Healthcare data migration must adhere to strict rules and regulations. HIPAA, GDPR, and regional health laws all apply. According to IBM, the average cost of a healthcare data breach is $10.93 million.
During migration, data is especially vulnerable if proper encryption, audit logging, and role-based access controls are not enforced.
4. Downtime and Clinical Workflow Interruption
System downtime during migration can directly impact patient care and clinical decision-making. Research shows that EHR downtime can result in up to 30% loss of clinician productivity and patient treatment delays.
Planning for minimum downtime requires parallel system operation, a lot of testing, and clear rollback strategies. All of this adds complexity to migration projects.
5. Scalability and Performance Limitations
Healthcare organizations are faced with exploding volumes of data. Imaging, genomics, wearables, and remote patient monitoring all contribute to this growth. IDC estimates that the rate of healthcare data growth is approximately 36% per year.
As mentioned earlier, migrating huge amounts of data while maintaining system performance and facilitating real-time clinical access is a major technical challenge.
6. Change Management and User Adoption
Successful data migration requires a change in the mindset of the clinicians and staff. Their adaptation to the new system matters. Changes in workflows, presentation of data, and system navigation may cause resistance if users are not properly trained.
Industry studies show that nearly 70% of healthcare digital transformation endeavors face adoption challenges. Poor training and usability issues are often the cause.
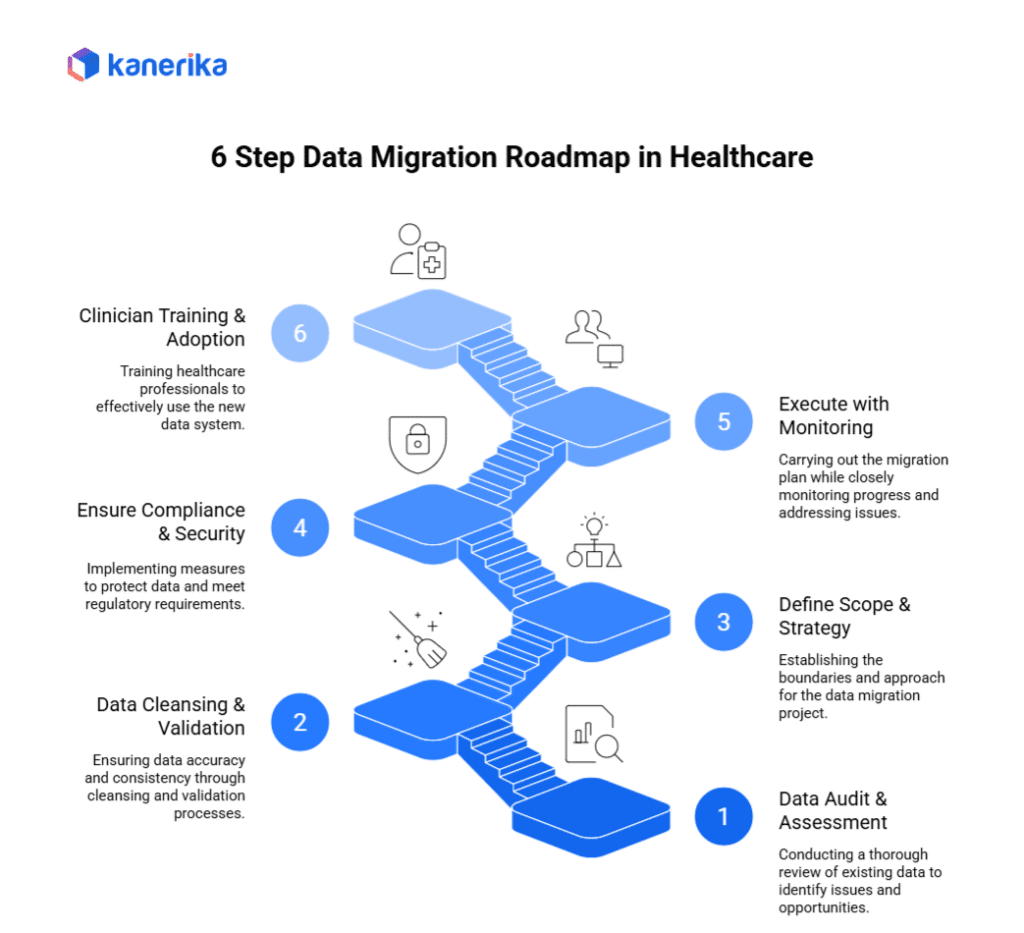
6-Step Migration Roadmap for Successful Healthcare Data Migration
Moving healthcare data from legacy systems to new systems requires careful planning and execution. These six steps provide a clear path to get it done right while keeping risks and disruptions to a minimum.
Step 1: Conduct a Comprehensive Data Audit and Assessment
Start every migration project with a good inventory of existing data sources, formats, and quality levels. Catalog all systems such as EHRs, imaging platforms, laboratory systems, departmental applications, and more to understand the full extent of data to be migrated.
Evaluate data relationships, dependencies, and integration points between systems. This foundation avoids surprises during the migration process and helps estimate realistic timelines and resource requirements for successful completion.
Step 2: Cleanse and Validate Data Before Migration
Invest in data quality improvement before starting the migration process. Work to remove duplicate patient records, standardize naming conventions, correct formatting inconsistencies, and fill critical data gaps where possible. Clean data leads to more reliable migrations with fewer post-migration problems.
Introduce validation rules to ensure data accuracy during the cleansing process. This is a big upfront investment, but it makes a huge difference by reducing the complications of migration and improving the quality of the target system from the first day.
Step 3: Define Overall Clear Scope and Decide Migration Strategy
Simply determine whether a big bang or phased migration is a better fit for organizational needs and the level of risk you are willing to take. Big bang migrations get done faster but come with a greater risk of widespread disruption. Phased approaches have less risk but involve longer transition periods and temporary system integration.
Consider factors like system criticality, user capacity for change, budget constraints, and regulatory requirements when choosing a strategy. Create detailed planning timelines of the project with realistic milestones and contingency plans for potential setbacks.
Cognos vs Power BI: A Complete Comparison and Migration Roadmap
A comprehensive guide comparing Cognos and Power BI, highlighting key differences, benefits, and a step-by-step migration roadmap for enterprises looking to modernize their analytics.
Step 4: Ensure Strong Compliance and Security
Build HIPAA and GDPR compliance into any aspect of the migration process. Implement end-to-end encryption for data in transit and data at rest, implement role-based access controls, and maintain detailed audit logs for the entire project.
Conduct routine compliance assessments and security reviews to identify vulnerabilities before they become violations. Work with legal and compliance teams to ensure that all of the migration activities are within regulatory requirements.
Step 5: Put Monitoring and Rollback Mechanisms in Place
Establish real-time monitoring systems to track migration progress and data integrity, as well as system performance during the course of the project. Create automated alerts for anomalies or failures that need immediate attention.
Develop complete rollback procedures to quickly restore the system to prior states in case critical issues occur. Test these procedures thoroughly before starting production migrations to ensure they work under the pressure of production.
Step 6: Engage Clinicians and Staff for Smooth Adoption
Involve clinical staff in migration planning to understand the impact on workflow and to collect input on system design decisions. Provide thorough training not only on the procedures themselves but also on how changes will improve patient care and operations.
Develop change management programs that address staff concerns, clearly communicate the benefits, and provide ongoing support during the transition period. As a result, successful adoption relies on user buy-in and confidence in the new systems.
Following these best practices minimizes the risks associated with migration, compliance with regulations, and creates sustainable foundations for modern healthcare technology platforms that improve the delivery of patient care.
Tools & Technologies for Healthcare Data Migration
1. Cloud Platforms: Healthcare-Specific Infrastructure
- AWS HealthLake provides a FHIR-compliant data lake designed specifically for healthcare organizations. It automatically transforms, indexes, and structures health data while maintaining industry standards for interoperability and security.
- Microsoft Azure for Healthcare offers comprehensive cloud services with built-in HIPAA compliance, including secure data storage, analytics capabilities, and API management specifically designed for healthcare workflows.
- Google Cloud Healthcare API enables healthcare organizations to store, process, and analyze medical data in real-time while maintaining strict privacy controls and enabling machine learning applications.
2. ETL Tools: Data Integration Specialists
- Informatica provides enterprise-grade data integration with sophisticated transformation capabilities and built-in data quality features essential for healthcare data migration projects.
- Talend offers open-source data integration solutions that provide cost-effective alternatives for organizations with budget constraints while maintaining professional-grade functionality.
- Fivetran automates data pipeline creation with pre-built connectors for healthcare systems, eliminating manual coding and reducing implementation time from months to weeks.
- Matillion delivers cloud-native ETL solutions that scale automatically with data volumes and integrate seamlessly with major cloud platforms.
3. EHR Migration Platforms: Specialized Healthcare Solutions
- Epic migration tools provide specialized capabilities for transitioning between Epic environments or migrating data from other systems into Epic, maintaining clinical workflow continuity.
- Cerner migration platforms offer purpose-built solutions for clinical data conversion that understand healthcare-specific data relationships and regulatory requirements.
4. Advanced Technologies: AI and Blockchain
- AI/ML data mapping automates the complex process of field mapping across different healthcare systems, reducing manual effort by 60-80% while improving accuracy through pattern recognition and machine learning.
- Blockchain technology creates immutable audit trails for migration activities, providing tamper-proof compliance documentation and ensuring data integrity throughout the transfer process.
These technologies work together to create comprehensive migration solutions that address healthcare’s unique requirements for security, compliance, and data integrity while minimizing disruption to patient care operations.
Case Studies: How Top Healthcare Providers Executed Large‑Scale Data Migrations
Case Study 1: Aurora Health Care: Large‑Scale Cerner to Epic Migration
Challenge
Aurora Health Care needed to migrate 32 terabytes of legacy clinical records, 75 terabytes of medical images, and 34 million scanned documents from Cerner Millennium to Epic. The AIX and Oracle 8 platform was reaching the end of life, creating urgent pressure to retire the system before support ended.
Solution
Aurora worked with Harmony Healthcare IT to build a high‑capacity healthcare archive. The archive maintained user access controls, preserved upstream and downstream system connections, and provided a simple interface that reduced training needs for clinical and administrative users.
Results
- 100% of reports migrated successfully on time and within budget.
- Significant reduction in legacy system maintenance costs.
- IT labor savings redirected to Epic rollout activities.
- Archive performance exceeded initial expectations.
Case Study 2: UPMC: Enterprise‑Wide Epic EHR Consolidation
Challenge
UPMC operated nine independent electronic health record systems across its 40 hospitals and 800 outpatient sites. Oracle Cerner supported inpatient care, and Epic supported outpatient workflows. This fragmentation required processing 27 million daily ADT messages, complicating care coordination and slowing clinical decision‑making.
Solution
UPMC began consolidating all systems into a single Epic platform. The transition includes moving six million patient medical records and coordinating a project team of 600 IT professionals and 1,200 clinicians across multiple specialties and care settings.
Results
- Expected to self‑fund within seven years through efficiency gains.
- Clinicians will gain instant access to complete patient histories.
- System complexity will drop sharply as nine platforms converge into a single platform.
- Improved continuity of care across inpatient and outpatient environments.
Case Study 3: AdventHealth: Cerner to Epic Migration for Enterprise Reporting
Challenge
AdventHealth needed to convert dozens of mission‑critical reports across revenue cycle, population health, and clinical operations. Cerner and Epic used different data models and workflows, making gap analysis and mapping extensive and complex.
Solution
SEHA Consulting worked with AdventHealth to design a comprehensive migration plan that covered data analysis, source-to-target mapping, new report creation, validation, and system-wide user training. The initiative aligned technical changes with clinical and operational workflows.
Results
- Zero disruption to clinical or business operations during transition.
- 100% of reports were migrated on time and on budget.
- Part of a 660 million dollar modernization initiative.
- Unified reporting structure across all hospitals and outpatient sites.
How to Migrate from SSRS to Power BI: Enterprise Migration Roadmap
Discover a structured approach to migrating from SSRS to Power BI, enhancing reporting, interactivity, and cloud scalability for enterprise analytics.
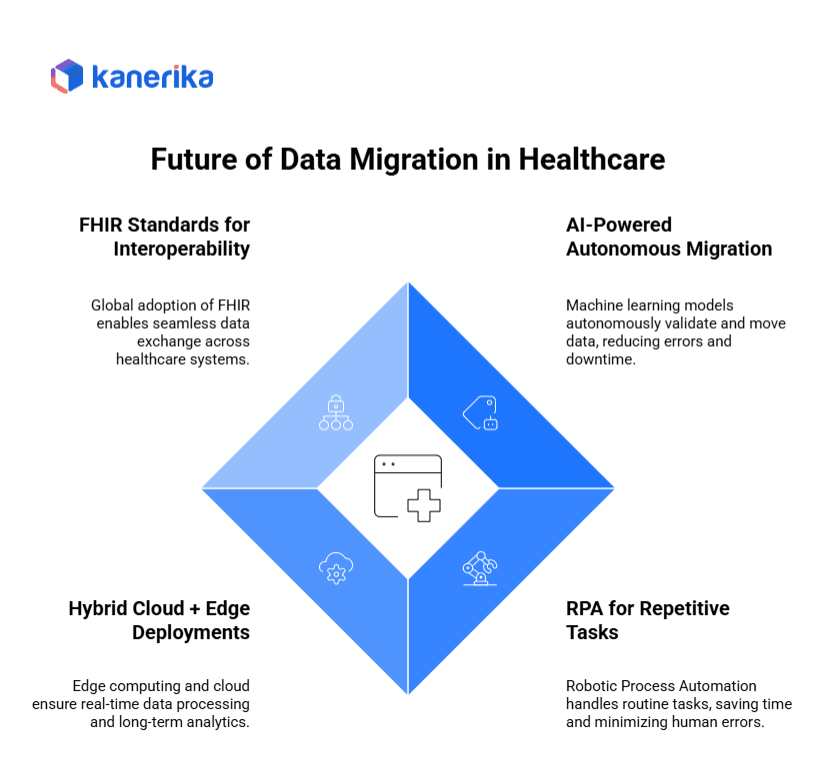
The Future of Data Migration in the Healthcare Industry
Data migration in healthcare is a rapidly changing game. Advanced technologies are pushing the industry beyond simple data transfer. Hospitals and providers are trending toward intelligent, automated systems that ensure continuity, compliance, and innovation.
1. AI-Driven Autonomous Migration
Machine learning models will be used to validate and clean data, and to move data with minimal human input. These systems can be used to detect anomalies and resolve duplicate records, and to dynamically ensure compliance. The result is fewer errors and less time spent. Healthcare teams will be spending less time on manual data handling and more time on patient care.
2. RPA for Repetitive Tasks
Robotic Process Automation will help with repetitive workflows such as claims transfer, record validation, and bulk uploads. By automating routine tasks, healthcare teams can save significant time. Human fatigue and errors drop when humans take over tedious work from machines. Staff can focus on tasks that require judgment and empathy.
3. Hybrid Cloud and Edge Implementations
The combination of edge and cloud helps in the real-time processing of patient data. In wearables, IoT devices, and hospital monitors, data processing will occur locally, facilitating instant insights. At the same time, data syncs with a secure cloud environment for long-term analytics. This hybrid approach is a compromise between speed and storage capacity.
4. FHIR Standards for Interoperability
The worldwide adoption of Fast Healthcare Interoperability Resources will allow seamless data exchange between various EHRs, insurers, and providers. FHIR standards will help break down silos and achieve true interoperability across the world’s healthcare ecosystems. Patient records will allow people to follow their care from provider to provider without friction.
5. Long-Term Vision Patient-Centric Ecosystems
Looking ahead, data migration will enable fully connected, patient-centric digital ecosystems. Every stakeholder, including patients, providers, insurers, and regulators, will securely access and update real-time data. This connected approach will be the driving factor for preventive care, population health management, and precision medicine. Healthcare will be more proactive and not reactive.
Kanerika: Simplifying Data Migration for Businesses Worldwide
Kanerika helps healthcare organizations move from legacy systems and silos to a modern, secure data platform. The goal is to make this transition without disrupting clinical or operational processes. Healthcare data is complex, high-volume, and highly regulated. This means migrations must be accurate and well-protected.
We develop data integrity migration schemes to ensure compliance with standards such as HIPAA and GDPR. Patient records, clinical data, and operational systems are smoothly moved into their new environments. Our team collaborates with hospitals, life sciences companies, diagnostic networks, and healthcare tech providers.
Our work covers several important areas. We consolidate EHR data and unify scattered clinical systems. We also handle on-premises workload migration to the cloud, including Azure, AWS, and Google Cloud. Automated migration accelerators and validation frameworks minimize manual effort and downtime. Every piece of data, from lab results to claim histories, remains accurate and traceable. This helps healthcare organizations reduce technical debt and improve the reliability of their data infrastructure.
Beyond migration, we ensure healthcare teams can get maximum benefit from their modernized systems. We optimize data models for analytics and enable real-time reporting. We also develop governance frameworks for better data quality and security. With Kanerika, healthcare providers receive more than a clean migration. They get a foundation for clinical decision support, AI-driven patient insights, operational efficiency, and long-term digital transformation.
SSIS to Fabric Migration Made Easy: A Complete Walkthrough
Learn how to migrate from SSIS to Fabric, streamline data integration, and enhance performance with this step-by-step walkthrough.
FAQs
1. What is healthcare data migration?
Healthcare data migration is the process of transferring patient records, EMRs/EHRs, billing, and clinical data from one system to another. This may involve moving from legacy systems to modern EHR platforms, on-premises to cloud, or consolidating data across providers for interoperability.
2. Why is data migration critical in healthcare?
Without smooth migration, patient care can be disrupted. Data migration ensures continuity of treatment, accurate patient histories, and secure access to records. It also helps organizations modernize infrastructure, comply with regulations, and reduce long-term IT costs.
3. How long does a typical healthcare migration take?
Timelines vary based on data volume, complexity, and compliance checks. Small migrations may take weeks, while large-scale hospital network migrations can last 12–24 months. Proper planning, phased rollouts, and pilot testing help speed up timelines without risking patient safety.
4. What are the risks of migrating healthcare data?
Common risks include data loss, duplication, security breaches, and system downtime. Poorly executed migrations may also lead to non-compliance with HIPAA or GDPR. Mitigating risks requires pre-migration audits, validation protocols, encryption, and rollback mechanisms.
5. Which regulations apply to healthcare data migration?
In the U.S., HIPAA governs the protection of patient data. Globally, GDPR (Europe), and other local regulations apply. Healthcare providers must also comply with standards like HL7 and FHIR to ensure interoperability and data security during migration.
6. What tools are best for EHR migration?
Tools like Mirth Connect, Talend, Informatica, AWS Healthcare Data Migration Services, and native vendor migration solutions (Epic, Cerner, Allscripts) are commonly used. The right tool depends on the size of the data set, compliance requirements, and integration needs.
7. How can hospitals ensure patient data accuracy during migration?
Accuracy requires data cleansing, validation, and testing at each stage. Automated reconciliation tools, pilot runs, and clinician involvement ensure that migrated data is consistent, complete, and usable. Regular audits post-migration help verify accuracy in live environments.











